
.avif)
Billing is the financial backbone of every ABA practice. AlohaABA’s billing software is built directly into the core of your practice management system, connecting appointments, clinical documentation, authorizations, and insurance claims into one seamless workflow. By reducing manual entry and increasing visibility across the revenue cycle, practices can reduce denials, improve clean claim rates, and strengthen overall financial performance.
.avif)
.avif)
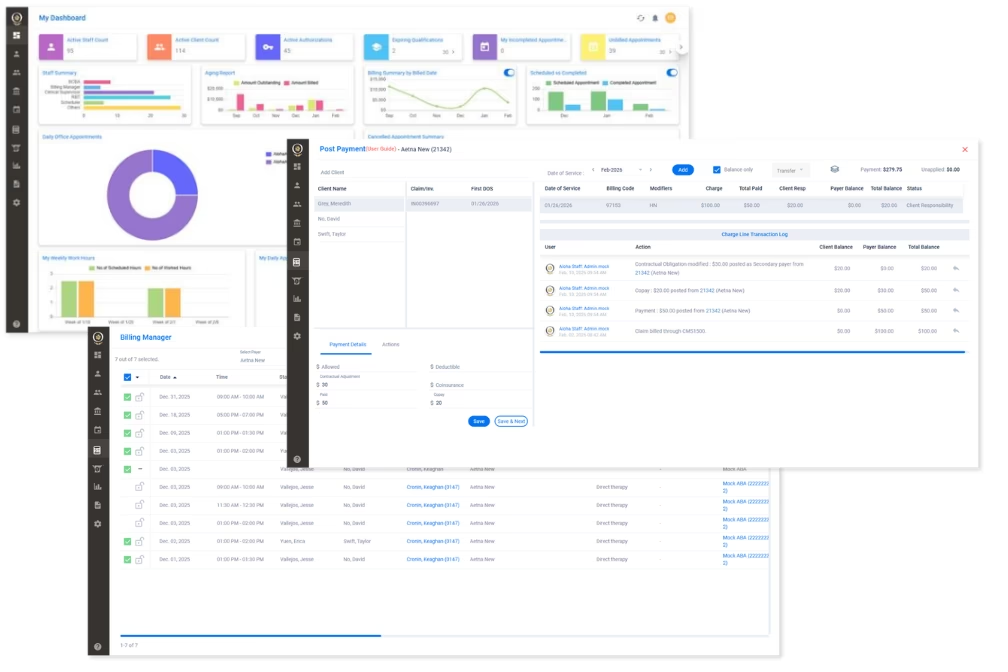
Track claims and payments using AlohaABA’s billing software, which keeps ABA providers informed every step of the way.With AlohaABA therapy management software, you can easily track claims and stay on top of revenue cycle management.
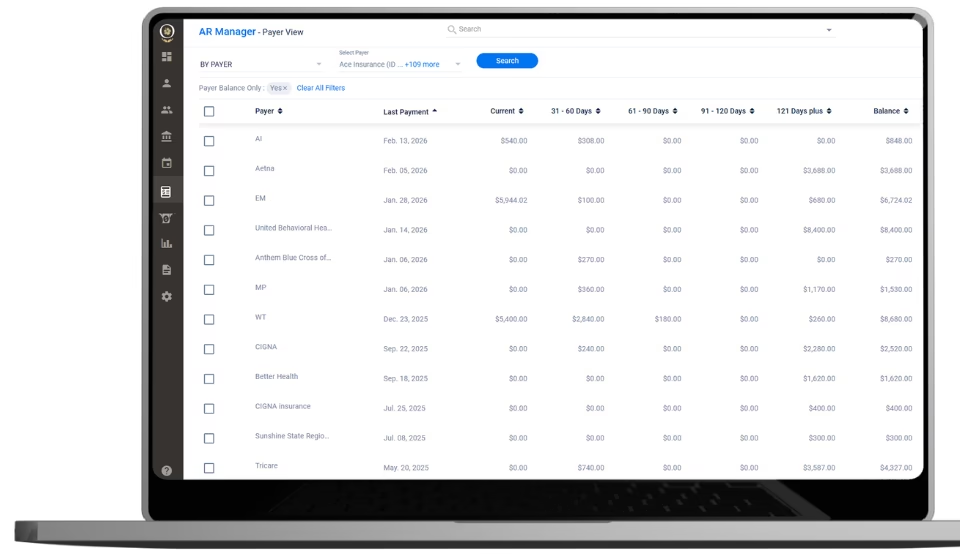
Our ABA billing software is consolidated to include claim tracking and accounts receivable which can be managed using AlohaABA’s AR Manager.





